Part 1
The conference room at St. Michael’s Hospital was the kind of place that smelled faintly of coffee, antiseptic, and overconfidence.
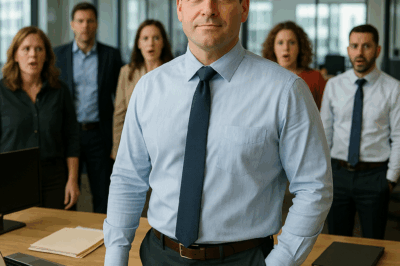
Nine specialists sat around the long walnut table—each a master of their field, each surrounded by binders, charts, and the smug certainty that came with years of letters trailing their names. Infectious disease, neurology, cardiology, gastroenterology, hematology, rheumatology, pulmonology, nephrology, endocrinology—every discipline represented.
And yet, they were all staring at the same lab results, equally baffled.
“Six weeks of persistent fever,” said Dr. Richard Hammond, the hospital’s chief of medicine. His voice was measured but strained. “Multiple organ involvement. No response to broad-spectrum antibiotics. No clear infectious, autoimmune, or malignant markers. We’ve run everything from hepatitis panels to full-body PET scans, and we’re still in the dark.”
Around the table, frustration hung like static. The sound of pages turning and pens clicking filled the silence that followed.
Sophie Parker stood at the back of the room, silent, unnoticed—a 26-year-old nurse with a clipboard pressed against her chest and a face that made her look barely out of college. She’d been present for nearly every consultation on James Whitmore’s case, watching the country’s top specialists argue in circles while the patient wasted away upstairs.
“Could be atypical lymphoma,” said Dr. Chen, hematology.
“We biopsied three sites,” countered Dr. Williams, oncology. “All negative.”
“Vasculitis panel?” offered Dr. Rodriguez, rheumatology.
“Negative,” Hammond replied, his tone tight. “Twice.”
Sophie shifted her weight, trying not to attract attention. But as she did, the movement caught Hammond’s eye.
“Nurse Parker,” he said, glancing up from his notes. “Do you need something?”
Nine pairs of eyes turned toward her. Some curious. Most annoyed.
She hesitated. Her pulse pounded in her throat. She shouldn’t—she couldn’t—interrupt. But Whitmore was dying, and no one was saying what needed to be said.
“No, Dr. Hammond,” she said, voice shaking slightly. “I just… I think I might know what he has.”
The silence was instant and absolute.
Dr. Hammond’s brows lifted slightly. “You think you know what he has? The patient nine specialists haven’t been able to diagnose?”
Sophie nodded. “Yes, sir. I believe I do.”
A soft chuckle came from Dr. Peterson, infectious disease. “Nurse Parker,” he said kindly but condescendingly, “we appreciate your enthusiasm, but this is an extremely complex case—one requiring years of specialized training to understand.”
“I understand that, doctor,” Sophie said. “But if you just look at—”
Hammond cut her off with a polite but firm smile. “We have this under control, Nurse Parker. Why don’t you check on Mr. Davis’s vitals and make sure his IV is running properly?”
Her cheeks burned. “Dr. Hammond, I really think—”
“That’s all, Nurse Parker. Thank you.”
It wasn’t a suggestion.
The room shifted uncomfortably. Someone coughed. Someone else whispered something she couldn’t quite catch, but she heard the word cute.
Sophie nodded stiffly, turned, and left the room.
As the heavy conference room door closed behind her, the laughter started—quiet, contained, professional—but laughter all the same.
“Thinks watching House M.D. makes her a diagnostician,” someone muttered.
“She’s ambitious,” another said. “Give her that.”
Sophie’s jaw tightened. They could laugh all they wanted—she knew. Every symptom fit. Every lab result, every clinical clue.
She knew exactly what James Whitmore had.
And every hour they wasted meant another piece of him was slipping away.
She found him in Room 417, the pale, feverish figure of a man who’d once been strong. His hair was damp with sweat, his skin sallow, his pulse weak beneath her fingers. The monitors hummed softly in the background—a mechanical heartbeat marking time he didn’t have.
“Mr. Whitmore,” she said gently, brushing the damp hair from his forehead. “I’m Sophie, one of your nurses. How are you feeling?”
He smiled weakly. “Like hell. Still no answers?”
“Not yet,” she said, checking his IV line. “But I wanted to ask you something—about your trip last year. You mentioned South America, right?”
His eyes fluttered. “Yeah. Brazil. Mission work. Six months.”
She leaned closer. “Did you spend time in rural areas? Near rivers or forests?”
“Villages,” he murmured. “Amazon basin. Why?”
“Just trying to understand your history better,” she said softly. “You rest now.”
She stepped out into the hallway, heart pounding. She knew. She knew.
Her mind raced as she pulled up medical databases on her phone, confirming what instinct and experience had already told her. Fever, hepatosplenomegaly, cardiac involvement, rash, neurological signs—it all fit.
Chagas disease.
It was rare in the U.S.—so rare most doctors would never see a case in their careers. But she’d seen it before. Dozens of times.
Because Sophie Parker hadn’t grown up like most nurses.
She’d spent twelve years of her childhood in Central and South America while her parents worked as medical missionaries. She’d helped treat patients in jungle clinics, learned the symptoms of tropical illnesses before she could drive, and had watched her father diagnose Trypanosoma cruzi infections in dusty field hospitals where textbooks were a luxury.
She didn’t need a textbook to recognize it now.
The only question was how to make anyone listen.
Twenty-four hours later, Whitmore was worse.
His liver enzymes were climbing, his kidneys failing, his cardiac rhythm unstable. The specialists were panicking—quietly, professionally—but panicking nonetheless.
Sophie had tried three times to raise her theory. Once with the attending. Once with Hammond directly. Once by leaving a note in Whitmore’s chart.
All three had been ignored.
Her supervisor, Linda Chen, found her at the nurses’ station, concern etched across her face.
“I heard you’ve been suggesting diagnoses to the specialists,” Linda said.
Sophie’s jaw tightened. “I know what he has, Linda. I’m certain.”
“Sophie…” Linda sighed. “I know you’re dedicated. But these are nine of the best specialists in the state. If they can’t figure it out, what makes you think—”
“I’ve seen it before,” Sophie interrupted—and immediately regretted it.
Linda’s eyebrows rose. “You’ve seen this before? Sophie, you’ve been a nurse for four years. Where exactly have you seen a case that’s baffling doctors with decades of experience?”
Sophie hesitated. She couldn’t tell her. Not without sounding delusional. Not without opening a part of her past she’d worked years to keep private.
“I… I read about it,” she said weakly.
Linda sighed again. “Look. I get it. You want to help. But Hammond called me personally. He asked that you stop interrupting their rounds with amateur theories. You’re a good nurse. Stick to what you’re trained for.”
And with that, she walked away.
Sophie stared through the glass at Whitmore’s room. His oxygen saturation was dropping. His temperature was 104.2. The “trial” of high-dose steroids the specialists were trying was making things worse, not better.
He was dying.
And she was the only one who knew why.
Something inside her hardened.
Rules or no rules, hierarchy or not—she wasn’t going to stand by and let a man die because she didn’t have the right title on her badge.
She walked into Whitmore’s room, past the specialists murmuring among themselves, and began checking his vitals. But what she was really doing was looking.
For one thing.
The mark.
And there it was—on the back of his neck, nearly hidden by his hair. Faint, circular, faded now but unmistakable to anyone who’d seen it before.
Her breath caught.
She was right.
Absolutely, undeniably right.
She turned to Dr. Hammond, her voice louder than usual.
“Dr. Hammond,” she said, “I need to show you something.”
He frowned, irritation flickering across his face. “Nurse Parker, we’ve been over this—”
“Please,” she said, forcing herself to hold her ground. “Just look. The back of his neck.”
Hammond sighed, humoring her. “Fine.”
She lifted the patient’s head gently, brushing the hair aside to reveal the faint circular mark.
“A small scar,” Hammond said. “Probably from childhood. Not relevant to—”
“It’s not a scar,” Sophie interrupted. “It’s a bite mark. From a triatomine bug.”
He blinked. “A what?”
“A kissing bug,” she said, her heart hammering. “If I’m right, Mr. Whitmore doesn’t have a mystery illness. He has Chagas disease.”
The room fell silent.
Then came the laughter.
“Chagas disease?” Dr. Peterson said incredulously. “That’s a tropical parasitic infection. This patient hasn’t—”
“He spent six months in rural Brazil last year,” Sophie said firmly. “In villages along the Amazon basin—exactly where triatomine bugs are endemic. The disease has an acute phase most people never notice. The chronic phase can appear years later with cardiac, gastrointestinal, and neurological symptoms.”
She pulled up images on the computer, hands shaking slightly. “His symptoms match perfectly. The cardiac involvement, the megacolon, the neurological signs. Everything. This bite mark is consistent with triatomine exposure.”
Hammond stared at the mark, then at her. “Chagas presents with specific cardiac findings. If you’re wrong—”
“Then test him,” Sophie said. “Serological testing for Trypanosoma cruzi. It’s a simple blood test. If I’m wrong, you lose a few hours. If I’m right, you can start treatment immediately and save his life.”
The room buzzed with murmurs. Calculations. Pride versus probability.
Dr. Rodriguez scoffed. “We’re not basing a treatment plan on the speculation of a nurse who—”
“Order the test,” Hammond said quietly.
Everyone turned to stare at him.
“Order the test,” he repeated. “Her theory is implausible—but it’s specific and testable. And if there’s even a one percent chance she’s right, we need to know.”
Sophie stood frozen as the specialists filed out, muttering under their breath.
“Waste of time.”
“Encouraging nurses to play doctor.”
“When it’s negative, someone needs to talk to her about boundaries.”
But Hammond’s eyes lingered on Sophie a moment longer before he left.
“If you’re right,” he said, “we’ll owe you an apology.”
She nodded once. “You will.”
Then she turned back to Whitmore, adjusted his blankets, and whispered under her breath—
“Hold on. Just hold on.”
Part 2
The serology test for Trypanosoma cruzi would take forty-eight hours.
James Whitmore didn’t have forty-eight hours.
By the next morning, his condition had plummeted. His liver enzymes were through the roof, his kidneys shutting down, his cardiac rhythm erratic enough that the monitors kept screaming false codes.
Sophie had been up all night.
She couldn’t leave his side, not when she knew what was happening inside his body—the parasites slowly tearing through his organs while nine experts debated theories that would never fit.
At 7:00 a.m., she finished charting his vitals when her phone buzzed.
Linda Chen: Hammond wants to see you. His office. Now.
Sophie stared at the text for a long second.
It was happening.
Her heart sank as she walked toward the administrative wing. Every step felt heavier, like the floor was preparing to swallow her whole.
Dr. Hammond’s office was large, sterile, and intimidating. The blinds were drawn, the morning light filtered through beige slats that painted stripes across the desk.
Hammond was sitting behind it, expression unreadable.
Beside him sat Dr. Patricia Morrison, the hospital’s chief of staff—polished, composed, the kind of woman who could fire someone with perfect diction and zero hesitation.
“Nurse Parker,” Morrison said coolly, “please, have a seat.”
Sophie sat, her palms damp against her scrubs.
“We’ve reviewed your personnel file,” Morrison began. “Four years of excellent performance reviews. No disciplinary history. Which makes yesterday’s behavior all the more… puzzling.”
“I was trying to help,” Sophie said. “I believe Mr. Whitmore has—”
“We know what you believe,” Hammond interrupted. “The question is why you believe it.”
He leaned forward, elbows on the desk. “Dr. Peterson did some research after your… suggestion. Chagas disease is exceedingly rare in the United States. Fewer than three hundred thousand known cases. Most physicians will go their entire careers without seeing one. So I need you to explain, Nurse Parker—how does a 26-year-old nurse with four years of experience recognize something nine specialists didn’t even consider?”
Sophie hesitated.
The truth wasn’t on her résumé. It was written into her childhood.
She took a slow breath. “Because I’ve seen it before,” she said quietly.
Morrison’s brow arched. “You’ve seen Chagas disease?”
“Yes, ma’am. Many times.”
“And where, exactly, did you see this?”
Sophie’s voice was steady now. “My parents are doctors. Medical missionaries. I grew up in developing countries—mostly in Central and South America. From age six to eighteen, I lived in villages where tropical diseases were part of everyday life. Chagas, dengue, leishmaniasis, schistosomiasis—I saw them all. I helped my parents in clinics. I learned to recognize the signs long before I ever went to nursing school.”
She took out her phone, scrolled to old photos.
“This is me at fourteen,” she said, showing a picture of herself in a dirt-floor clinic in Paraguay, surrounded by locals and makeshift medical equipment. “We saw Chagas cases almost weekly.”
Another photo—Bolivia, age sixteen. “My father used to show me the marks. The bite pattern. The facial swelling that fades but leaves cardiac scarring. I’ll never forget it.”
Morrison leaned forward, studying the images. The silence stretched, thick and heavy.
Finally, Hammond spoke. “So when you saw Whitmore’s chart—his travel to Brazil, his multi-system involvement—you recognized the pattern immediately.”
Sophie nodded. “Yes, sir. Everything fit. The cardiac issues, the GI symptoms, the neurological involvement. And when I saw that bite mark…” She met his gaze. “I knew.”
Morrison set her pen down. “Why didn’t you mention your background before?”
Sophie hesitated. “Because it’s not part of my official credentials. Because I’ve spent four years trying to be taken seriously as a professional. And admitting I learned medical knowledge from a jungle clinic when I was a teenager doesn’t exactly inspire confidence in people who think expertise only comes with degrees.”
Her voice wavered—but she didn’t back down. “And because I knew no one would listen.”
For a moment, no one spoke. The clock on Hammond’s wall ticked softly, each second stretching the silence thinner.
Then Hammond said, “The test results came back early.”
Sophie’s heart stuttered. “What?”
He looked at her, voice low. “Preliminary results are positive for Trypanosoma cruzi antibodies.”
She froze. “Positive?”
He nodded slowly. “Mr. Whitmore has Chagas disease.”
The air left her lungs all at once. Relief flooded through her so quickly it was almost dizzying.
“Can we start treatment?” she asked breathlessly. “Benznidazole or nifurtimox?”
“Already being initiated,” Morrison said. “We consulted with the CDC this morning. They confirmed your diagnosis and sent us the treatment protocol.”
For a long moment, Sophie couldn’t speak. The rush of relief, disbelief, vindication—all tangled together until she could only whisper, “He’s going to live.”
“Yes,” Hammond said. “He’s going to live.”
Morrison stood. “Sophie, you saved that man’s life. If you hadn’t recognized the disease—if you hadn’t pushed—we’d have lost him within days.”
Hammond’s tone softened, but not without edge. “You also violated several protocols, challenged attending physicians in front of staff, and bypassed chain of command.”
Morrison shot him a sharp glance. “She did what any competent healthcare professional should do when they have critical information—she spoke up. Even when it was uncomfortable.”
Sophie blinked, unsure whether she was being praised or reprimanded.
Morrison smiled faintly. “I’m not going to discipline you. I’m going to thank you. And I’m going to make sure everyone here understands that good ideas don’t come with job titles attached.”
Hammond sighed, conceding with a nod. “You’ll return to your regular duties. But, Nurse Parker…” His eyes met hers. “Don’t ever let anyone’s dismissal stop you from speaking up again.”
“Yes, sir.”
She rose, still reeling.
As she left the office, she heard Morrison say softly, “We’ll need to revisit our interdisciplinary communication policy. She shouldn’t have had to fight this hard to be heard.”
When Sophie returned to the floor, the news hadn’t yet spread.
Whitmore was stable for the first time in days, his fever dropping, the faintest trace of color returning to his cheeks.
He opened his eyes as she entered. “Nurse Parker,” he rasped. “You look like you just ran a marathon.”
“Feels like I did,” she said with a shaky smile.
“The doctors said… you were the one who figured it out?”
She hesitated, modestly. “We all worked together.”
He studied her face. “You saved my life, didn’t you?”
Sophie blinked back tears. “I just did my job.”
“No,” he said. “You did more than that.”
The following morning, word spread like wildfire.
Nine specialists—each one formerly certain of their authority—now faced the uncomfortable truth that they had missed a diagnosis caught by a 26-year-old nurse.
Sophie heard fragments in the hallway.
“Lucky guess.”
“Still inappropriate.”
“Doesn’t change the hierarchy.”
She let it roll off her.
Because hierarchy hadn’t saved Whitmore.
Courage had.
Two days later, Hammond found her in the ICU hallway.
“Results are definitive,” he said. “Full serology confirmed. Mr. Whitmore’s responding well to treatment.”
Sophie smiled. “That’s good news.”
Hammond nodded, hesitated, then said quietly, “You were right, Nurse Parker. I owe you an apology.”
She was too stunned to respond.
He continued, “We all do. You saw what we didn’t. And you had the conviction to fight for it.”
“It wasn’t courage,” she said softly. “It was desperation.”
“Sometimes those are the same thing,” Hammond said. “Don’t lose that instinct.”
He paused, then added with a faint smile, “By the way, the specialists are presenting the case at Grand Rounds next week. I think you should be there.”
Her brows lifted. “To be mocked again?”
“To be credited,” Hammond said. “You made the call that saved a man’s life. People need to know that.”
He walked away before she could answer.
Sophie watched him go, her heart lighter than it had been in weeks.
She turned back toward Whitmore’s room, where the monitors hummed steady, rhythmic, alive.
And for the first time, she allowed herself to smile—not with pride, but with peace.
She’d been right.
He would live.
And maybe, just maybe, people were starting to listen.
Part 3
The following week at St. Michael’s Hospital felt like something had changed—only no one could quite admit it.
Rumors had spread fast. Everyone in the building knew that a young nurse had correctly diagnosed a patient nine senior specialists couldn’t. The story had traveled from the ICU to the cafeteria, from the night shift to the administration wing, growing in detail with every retelling.
Some called her lucky.
Some called her reckless.
But others—quietly, respectfully—called her brilliant.
Sophie Parker didn’t call herself anything.
She came in early, same as always, reviewed vitals, adjusted IV drips, charted medications. But the looks were different now. Nurses gave her nods of encouragement; residents offered her awkward, impressed smiles. Even a few physicians met her gaze instead of glancing past her like she was part of the wallpaper.
Whitmore was improving fast.
His fever gone.
His color returning.
The man who had been hours from multi-organ failure was now sitting upright, eating oatmeal and making bad jokes about hospital food.
“You must be some kind of genius,” he said, grinning as Sophie checked his blood pressure.
“I just paid attention,” she said, smiling softly.
“No,” he said, shaking his head. “You listened when no one else would. That’s rarer than genius.”
Sophie didn’t answer. She tightened the cuff, focusing on the rhythmic pulse beneath the fabric. It wasn’t just his heart that had started beating steady again—it was hers, too.
That afternoon, Dr. Hammond appeared at the doorway, followed by Dr. Peterson, Dr. Chen, and several other specialists from the case. They filled the room in their immaculate white coats, a silent storm of authority.
Whitmore straightened. “Ah, the dream team,” he said lightly.
“Mr. Whitmore,” Hammond began, “we wanted to check on your progress. I understand Nurse Parker has explained your diagnosis.”
Whitmore chuckled. “She didn’t just explain it. She saved me.”
Dr. Peterson cleared his throat, his voice measured but uneasy. “Yes, well, Nurse Parker’s observation was… indeed correct. Which brings us to why we’re here.”
He turned to Sophie. “Nurse Parker, we owe you an apology. A collective one.”
The room fell quiet.
Sophie froze, caught between disbelief and embarrassment.
“You were right,” Peterson continued. “Your diagnostic reasoning was sound. And we dismissed you—not because of your logic, but because of your position.”
Dr. Rodriguez, rheumatology, stepped forward next. “I’ve been a physician for thirty years. I’ve never encountered a single case of Chagas disease. I assumed my experience meant I knew better. I was wrong.”
Dr. Williams, oncology, spoke next. “We talk about evidence-based medicine, but what you showed us was something harder to teach—pattern recognition born of lived experience. We need to value that more.”
Sophie’s throat tightened. She wasn’t sure whether to speak or stay silent, so she did the only thing that felt natural—she nodded, eyes glistening.
“Thank you,” she said softly. “That means more than you know.”
Hammond smiled faintly. “We’d like you to present the case with us at next week’s Grand Rounds. Walk everyone through how this diagnosis was made—and what we can learn from it.”
Sophie blinked. “You want me to… present? In front of the entire hospital?”
“Yes,” Hammond said simply. “You caught what we missed. The lesson isn’t just about the disease—it’s about humility.”
Dr. Chen added, “We’ve also contacted the Journal of Diagnostic Medicine. They’re interested in publishing the case. They want you listed as lead author.”
The words hit her like a shock. Lead author.
Her. A nurse.
Her hands trembled slightly as she nodded. “I—I’d be honored.”
When they left, Whitmore laughed. “You’re famous now.”
Sophie shook her head. “No. Just lucky.”
“Luck doesn’t read scars,” Whitmore said quietly. “Luck doesn’t fight the system to save a stranger.”
The day of the Grand Rounds, Sophie’s hands wouldn’t stop shaking.
She stood backstage in the auditorium, a place usually reserved for renowned surgeons and visiting professors. Rows of seats filled with white coats, medical students, residents, administrators—all waiting to hear about the miracle diagnosis that had turned the hospital upside down.
Dr. Hammond joined her, offering a reassuring smile. “Nervous?”
“Terrified,” she admitted.
“You’re about to change how people here think,” Hammond said. “That’s supposed to be terrifying.”
The lights dimmed. The murmuring crowd fell silent.
Dr. Peterson began. “Today we’re presenting a complex diagnostic case: a 54-year-old male with fever of unknown origin, multi-organ involvement, and six weeks of failed interventions.”
He walked through the medical timeline—every test, every negative result, every dead end. The audience nodded, following the familiar pattern of diagnostic frustration.
Then Peterson paused, clicked the next slide, and said:
“The person who solved this case was not one of the nine specialists you see listed here.”
A low murmur rippled through the crowd.
“She was a nurse,” Peterson said, “with four years of experience. No medical degree. No specialty training. But what she did have was unique insight—born from life experience none of us possessed.”
He gestured toward the side of the stage. “Nurse Sophie Parker.”
Sophie stepped out. The applause startled her—it wasn’t thunderous, but it was warm, genuine, and unexpected.
She took the podium, heart pounding.
“When I first read Mr. Whitmore’s chart,” she began, “one detail stood out—his six-month mission trip to rural Brazil. To most physicians here, that was just background information. But to me, it was a red flag.”
She clicked through her slides. Photos of the triatomine bug. Maps of endemic regions. Clinical patterns. Cardiac involvement. Neurological symptoms.
“I grew up in Central and South America,” she said. “In the villages where I lived, diseases like Chagas were common. The presentation is distinct if you’ve seen it—but if you haven’t, it looks like a dozen other conditions.”
She showed an image of the bite mark. “This small circular lesion—barely noticeable. But to someone who’s seen it before, it’s diagnostic. I recognized it immediately.”
She paused, scanning the room. “This case isn’t just about one rare disease. It’s about what happens when we stop listening to each other. When hierarchy gets louder than curiosity.”
A hush fell over the auditorium.
She took a breath. “In medicine, we’re taught that when you hear hoofbeats, think horses, not zebras. But sometimes,” she said softly, “you need someone in the room who’s seen a zebra to tell you that’s what it is.”
For a moment, no one moved. Then, slowly, applause built—quiet at first, then growing until the room was filled with the sound of respect.
Dr. Williams rose from the front row. “I think we all owe Nurse Parker a thank you—for reminding us what medicine is supposed to be about: observation, collaboration, and humility.”
The applause doubled.
Sophie blinked hard, trying not to cry.
After the presentation, people surrounded her.
Medical students asking questions. Residents shaking her hand. Nurses hugging her.
One young medical student, maybe twenty-two, approached shyly. “I wanted to thank you,” she said. “I almost dropped out of med school because I kept feeling like my background didn’t belong here. But you just showed me it’s an advantage.”
Sophie smiled. “Never hide what makes you different. That’s where your strength is.”
Later, Dr. Hammond found her alone in the hallway, packing up her notes.
“You did well,” he said.
“Thank you,” she said quietly. “Though I think half the room was in shock that a nurse was at the podium.”
“They won’t be for long,” he replied. “You’ve started something. People are talking. Rethinking.”
He hesitated, then added, “Have you ever considered medical school?”
Sophie laughed softly. “After four years of being told to stay in my lane? I don’t know if I could survive the hierarchy.”
“You already have,” Hammond said with a grin. He handed her a business card. “My colleague runs a bridge program for nurses interested in becoming diagnostic practitioners or PAs. Think about it.”
She took the card, fingers brushing the embossed letters. “Maybe I will.”
That evening, Sophie sat alone in the hospital courtyard, the city lights glowing beyond the glass walls. The weight of the day finally caught up to her.
She wasn’t sure if she felt pride or exhaustion—or maybe both.
She thought about Whitmore, alive and smiling. About the laughter in that first meeting. About how hard it had been to say five simple words:
I know what he has.
Five words that had changed everything.
Part 4
A month after the Grand Rounds presentation, St. Michael’s Hospital felt different.
Not dramatically — no banners, no public statements, no overnight revolution — but quietly, like the slow shift of a current beneath the surface.
People listened more.
Residents asked nurses what they noticed during rounds. Attendings paused before dismissing ideas that didn’t come from their peers. And somewhere deep in the hospital’s culture, something old and rigid had begun to bend.
Sophie Parker never asked for credit. She didn’t need it. Every time she passed James Whitmore’s room and saw him sitting up, eating breakfast with a smile, she was reminded that the reward was already alive and breathing.
But the whispers of her story traveled farther than she could’ve imagined.
By spring, the hospital administration had started discussing a new pilot role — a diagnostic liaison nurse — a position that would allow experienced nurses to contribute directly to complex case reviews.
It was inspired, officially, by “recent interdisciplinary successes.”
Unofficially, everyone knew it was because of her.
On an ordinary Tuesday morning, Sophie sat in Director Patricia Morrison’s office, her hands wrapped around a mug of coffee that had gone cold.
Morrison leaned back in her chair, reading from a stack of papers. “You’ve been offered three positions,” she said. “A scholarship for the nurse practitioner program at Columbia, a consulting role in infectious disease here at St. Michael’s, and an invitation to join a global health initiative that trains clinicians in tropical disease recognition.”
Sophie blinked. “I… don’t even know how to process that.”
Morrison smiled. “That’s because you’re the first nurse in this hospital’s history to receive offers like this after a single case presentation.”
Sophie set the mug down. “I love patient care,” she said slowly. “I love being with people. But I also want to teach — to help doctors and nurses recognize diseases like Whitmore’s before it’s too late. I don’t want anyone else to go through that.”
Morrison nodded. “Then do both.”
“Both?”
“Stay in bedside nursing, but take on a dual role — a diagnostic liaison nurse. You’d handle patient care and consult on complex or undiagnosed cases. You’d be our test run for the new position.”
Sophie’s breath caught. “That’s… exactly what I want.”
“There’s one condition,” Morrison said. “You have to promise to keep speaking up. No hesitation. No hierarchy. If you see something, say something — even if you’re outnumbered nine to one.”
Sophie smiled faintly. “I can promise that.”
“Good,” Morrison said, standing. “And I’ll make the same promise for the physicians — that they’ll listen when you do.”
For the first time since this whole thing began, Sophie felt the ground under her feet start to level.
Two weeks later, Sophie was invited to speak at the National Nurses Association Conference in Chicago.
The ballroom was packed — hundreds of nurses, administrators, educators — the hum of anticipation filling the air like static. She stood behind the podium, the spotlights hot on her face, and took a deep breath.
“When I first started nursing,” she began, “I was told one thing more than any other: Know your place.”
A low murmur swept through the room — knowing, weary laughter from people who’d heard the same.
“I was taught to respect hierarchy. To trust that the doctors knew best. To follow protocol, even when my gut told me something was wrong.”
She paused, meeting the eyes of the audience.
“And for a long time, I did exactly that. Until one day, I couldn’t anymore.”
She told them about Whitmore — about the fever that wouldn’t break, the nine specialists, the laughter in the conference room, and the voice inside her that refused to be quiet.
“I knew what he had,” she said. “But every time I tried to speak up, I was told to stay in my lane. To remember my role. To let the experts handle it.”
She held the silence that followed.
“He would’ve died,” she said finally. “If I hadn’t spoken again. If I hadn’t broken the rule I’d been trained to obey.”
The crowd was completely still.
“This isn’t about me,” she continued, her voice steadier now. “It’s about all of us. Nurses see things others miss. We spend more time with patients than anyone. We hear what they don’t tell their doctors. We notice patterns, behaviors, tiny details that don’t fit. That’s knowledge. That’s expertise. But too often, it goes unheard because of our titles.”
She scanned the room. “I’m here to tell you — your instincts matter. Your voice matters. And when a patient’s life is on the line, speaking up isn’t overstepping. It’s your duty.”
The applause started slowly — one nurse, then another, then the whole room rising to its feet.
When Sophie stepped offstage, she was met by a stream of nurses — some young and idealistic, others seasoned and battle-worn.
One older nurse, gray hair pulled back in a bun, gripped Sophie’s hand tightly. “I’ve been doing this forty years,” she said, voice trembling. “I stopped speaking up a long time ago because I got tired of being ignored. But listening to you… you reminded me why I started nursing in the first place.”
Sophie swallowed hard. “Thank you,” she said softly.
The woman squeezed her hand. “No. Thank you.”
Months passed, and Sophie’s new role took shape. Her small office near the ER became a place of quiet miracles.
When complex or unexplained cases came in, doctors began calling her in for a second look. Sometimes her contribution was small — an observation, a question, a memory from her time overseas. But sometimes it was everything.
One morning, Dr. Hammond called her personally.
“Sophie, we’ve got a 38-year-old woman with a four-week fever of unknown origin,” he said. “Multiple specialists stumped. Can you take a look?”
Within minutes, Sophie was reviewing the chart.
Patient: Katherine Lewis.
Occupation: Pet store manager.
Pets: Two cats, adopted three months ago.
Sophie’s brow furrowed. “When did she adopt her cats?”
“Three months ago,” Hammond said, flipping pages. “Why?”
“Has anyone tested her for Bartonella henselae?”
Hammond paused. “Cat scratch disease?”
“Yes,” Sophie said. “It’s rare for it to present systemically, but atypical cases can cause prolonged fever, lymph node enlargement, even liver involvement. Everything in her labs fits.”
“Good catch,” Hammond said. “We’ll order the test.”
Two days later, the results came back positive.
Another mystery solved. Another life redirected.
When Hammond called to tell her, he laughed softly. “You’ve got a talent, Parker. You keep making the rest of us look bad.”
“I’m not trying to,” she said. “I just ask different questions.”
“Keep asking them,” he replied. “The hospital’s better for it.”
That evening, as Sophie packed up her things, a nervous-looking first-year nurse named Rachel approached her.
“Can I ask you something?” Rachel said.
“Of course.”
“I have a patient with pneumonia that isn’t responding to antibiotics. The doctors think it’s resistant bacteria, but he mentioned he works at a pet store — with birds. Could it be…?”
“Psittacosis,” Sophie finished. “Bird exposure, respiratory symptoms, poor response to beta-lactams — it fits. You should mention it.”
Rachel bit her lip. “I don’t want to sound like I’m telling them what to do.”
Sophie smiled. “You’re not telling them what to do. You’re sharing what you know. That’s the job.”
An hour later, Rachel returned, eyes wide. “They tested for psittacosis. It was positive. They’re starting the right antibiotics.”
Sophie grinned. “You see? You didn’t need me. You just needed permission to trust yourself.”
Late that night, Sophie sat alone in her small office, the hospital humming quietly around her. She thought about the path that had brought her here — from that humiliating conference room to this moment of quiet respect.
She thought about Whitmore, about every patient whose life had hinged on whether someone had the courage to speak.
She reached into her desk drawer and pulled out a photo — Whitmore’s family, smiling, healthy, alive. A note on the back read:
“For the nurse who saved my life — and reminded my family that miracles sometimes wear scrubs.”
Sophie traced the words with her thumb.
Five words had changed everything.
I know what he has.
Five words that had once cost her ridicule.
Five words that had now saved more lives than she could count.
And somewhere deep inside, she knew—
This was only the beginning.
Part 5
Two years after the case that had changed everything, the same conference room at St. Michael’s Hospital looked almost identical — same polished table, same faint hum of fluorescent lights — but the energy was completely different.
Back then, this room had been filled with skepticism, with laughter that hid insecurity, with nine specialists unwilling to hear five simple words from a nurse who looked too young to know what she knew.
Now, that same nurse stood at the head of the room.
Not as a subordinate.
Not as an observer.
But as the lead of a new national initiative.
Sophie Parker adjusted the microphone as hospital administrators, physicians, and nursing leaders filled the seats. Beside her stood five other nurses, each wearing badges that read Diagnostic Liaison Nurse — Founding Team.
Dr. Hammond opened the session.
“Two years ago,” he began, “a 54-year-old man named James Whitmore was admitted with a fever of unknown origin. Nine specialists — myself included — failed to identify the cause. It was a nurse, just four years into her career, who recognized the diagnosis and saved his life. That moment taught us something invaluable: that expertise doesn’t always come from where we expect it.”
He turned toward Sophie with a proud smile. “Today, we’re here to launch the Diagnostic Liaison Nurse Program — a model designed to integrate nursing insight directly into complex case diagnostics.”
Applause filled the room.
Sophie stepped forward. “Thank you, Dr. Hammond. And thank you to everyone who believed that change was possible.”
She clicked to the first slide: ‘The Problem: Diagnostic Hierarchy.’
“For too long,” she said, “medicine has been built on vertical lines — authority flowing one way, from top to bottom. But diagnosis isn’t linear. It’s collaborative. The more perspectives we include, the fewer things we miss.”
She clicked again. A graph appeared, showing the results of the pilot program.
“In the eighteen months since implementing this model, our hospitals have seen a 32% reduction in diagnostic delays for complex cases and a 41% increase in rare disease identification.”
She glanced around the room. “That’s not because nurses are smarter than doctors. It’s because we bring different data. We observe differently. We notice what others don’t.”
The next slide showed photos of the five nurses beside her — each responsible for catching life-saving details that had slipped through traditional systems.
“Nurse Patel recognized early-onset Addison’s in a patient misdiagnosed with depression.”
“Nurse Williams identified a severe allergic reaction disguised as pneumonia.”
“Nurse Ramirez diagnosed leptospirosis after a flood-zone rescue.”
“These nurses,” Sophie said, “proved that when every voice is valued, patients live.”
During the Q&A session, a hand rose in the back — Dr. Peterson, the infectious disease specialist who had once laughed at her two years ago.
“I was one of the nine,” he said, his voice steady but humble. “And I’ve spent the last two years asking myself why I dismissed you.”
The room went quiet.
“I realized it wasn’t arrogance,” he continued. “It was training. We’re taught that expertise equals credentials. That answers come from up the hierarchy, not across it. But this program — your program — showed me that’s not just wrong, it’s dangerous. I’m a better diagnostician today because I listen differently now.”
The applause that followed wasn’t polite; it was emotional, genuine. It wasn’t just about Sophie’s victory anymore. It was about an entire culture learning how to heal itself.
After the presentation, people gathered around Sophie — physicians asking how to implement the model in their hospitals, nurses thanking her for giving them a voice, residents telling her they’d never look at interdisciplinary rounds the same way again.
A young resident approached her shyly. “I want to be the kind of doctor who listens,” he said. “Who doesn’t dismiss nurses. How do I start?”
Sophie smiled. “Start by asking them what they think. When you’re stuck, ask your nurse what they’ve noticed. They’ve been watching longer than you have.”
He nodded, eyes bright. “Thank you.”
When the room finally emptied, Sophie stood by the window, looking down at the hospital courtyard.
Two years ago, she’d walked this same floor in humiliation, dismissed and ignored.
Now, the same walls echoed with her name.
Dr. Hammond joined her. “You realize,” he said, “you’ve changed how we practice medicine here. Maybe even beyond here.”
Sophie smiled softly. “All I did was speak up.”
Hammond shook his head. “No, Sophie. You spoke up and wouldn’t stop. That’s what changed things.”
He hesitated, then added, “Do you ever think about how different things would be if you hadn’t said those five words that day?”
She looked out the window, where the morning sun was climbing over the city.
“All the time,” she said quietly. “If I hadn’t said them, Whitmore would probably be dead. I’d still be scared to challenge anyone. The program wouldn’t exist. The other nurses wouldn’t have the courage to speak up. Five words changed everything.”
Hammond nodded. “That’s courage, Sophie — not the absence of fear, but speaking anyway.”
That evening, as the hospital lights dimmed, Sophie returned to her office — the same small space tucked beside the emergency wing, walls lined with case files and tropical disease references.
On her desk sat a frame she hadn’t noticed before.
Inside it, a photo — James Whitmore with his family, smiling, alive, holding up a sign that read:
“Thank you, Sophie — for giving us more time.”
Beneath it, a handwritten note:
“You didn’t just save my life. You changed how medicine listens. You gave meaning to every nurse who ever stayed quiet. We’ll never forget that.”
Her throat tightened. She traced the handwriting with her fingers.
The hospital PA crackled overhead: “Code blue, ER.”
Sophie stood immediately, grabbed her badge, and ran — her sneakers squeaking against the linoleum floors.
Down the hallway, through the sliding glass doors, back into the heart of the chaos she loved.
Because this was who she was. Not a title. Not a hero.
Just a nurse — the kind who noticed what others missed, who asked questions no one else thought to ask, who believed that listening could save lives.
Later that night, when the emergency had passed, Sophie walked back down the quiet hallway alone. The building was hushed again, lights dimmed, the hum of machines a soft lullaby.
She passed the conference room where it all began — that place of laughter and disbelief — and paused.
Through the glass, she saw her reflection. Not the same young woman from two years ago, not the girl with a clipboard pressed to her chest, afraid to speak.
This woman stood taller. Still humble, but unshakable.
She whispered to her reflection, almost smiling.
“I know what he has.”
The words no longer carried fear. They carried power.
Months later, the Diagnostic Liaison Nurse Program spread beyond St. Michael’s.
Dozens of hospitals adopted the model.
Medical schools began teaching modules on interdisciplinary humility.
The Journal of Diagnostic Medicine published a follow-up paper co-authored by Sophie and Hammond:
“The Power of Listening: Rethinking Expertise in Collaborative Diagnosis.”
It became required reading in nursing programs nationwide.
And in every lecture, every seminar, every hospital that discussed the case of James Whitmore, the same quote appeared on the first slide:
“Good medicine isn’t about who’s right. It’s about what’s true — and the courage to say it.” — Sophie Parker, RN
Two years after saving Whitmore, Sophie was invited to speak at a medical school commencement in Boston.
She stood before hundreds of graduating doctors and nurses, their white coats gleaming in the auditorium light.
“When you walk into your first patient’s room,” she said, “remember this: everyone you work with knows something you don’t. The janitor, the tech, the nurse. Listen to them. Respect them. Learn from them.”
She paused, her gaze steady. “And when you know something no one else sees — when the patient’s life depends on it — say it. Even if they laugh. Even if they call you naïve. Say it anyway. Because those five words might be the most important ones you’ll ever speak.”
Her voice softened. “I know what he has.”
When she stepped off the stage, she was met with a standing ovation — not just for her story, but for what it represented.
The idea that courage wasn’t a privilege.
It was a responsibility.
That night, back home, Sophie stood in her kitchen, watching the lights of the city flicker beyond the window.
She thought about Whitmore’s laugh. Rachel’s first success. The hundreds of nurses who now spoke up without fear. The thousands of patients whose lives would be changed because one young nurse refused to stay quiet.
She whispered softly to the empty room,
“That’s all it ever takes — one voice, one moment, five words.”
She smiled to herself.
And for the first time, the silence that followed didn’t feel heavy.
It felt like peace.
THE END
News
CH2 – Rich Teen Disrespects Judge Caprio in Court – His Response Is Pure Justice…
Part 1 The courtroom at Providence Municipal Court had seen its share of arrogance before—impatient businessmen, defiant drivers, even the…
CH2 – My Sister’s Kid Spat On My Birthday Cake And Yelled, “You Don’t Deserve It Anyway!” I Stayed Silent…
Part One: It happened on my thirty-fourth birthday. The living room was too warm, filled with the familiar clutter of…
CH2 – They Offered Newcomers 40% More Than Me After 9 Loyal Years; My Final Move Left Jaws Dropping…
Part One: There are moments in life when numbers stop being numbers — when they become confessions. That morning began…
CH2 – Woman Refuses to Hang Up Phone in Court — Judge Caprio’s Response Left Her in Handcuffs…
Part One: It was one of those crisp Providence mornings when the light filters through the courthouse windows like a…
CH2 – I USED MY SPARE KEY AND FOUND MY GRANDSON IN HIS CRIB, SCREAMING, UNCHANGED FOR HOURS…
Part 1 The first time I heard the baby cry that morning, I thought it was the TV. Some infomercial…
CH2 – When 12-year-old Aurelio saw the man in the expensive suit falling into the river, he didn’t know that this act of bravery would change not only the life of the city’s most powerful millionaire, but also his own destiny forever…
The midday sun scorched the streets of Ciudad de Esperanza, painting the city in a shimmer of heat and dust….
End of content
No more pages to load