Marcus sprinted through Metropolitan Hospital’s marble lobby, dodged two security guards, slipped past the reception desk, and burst through the ICU doors where a millionoll medical team had just declared 16-year-old Sophia’s case hopeless. Stop the treatment. You’re killing her,” the barefoot 12-year-old shouted, grabbing the patient chart from Dr. Elizabeth Whitmore’s hands. “This isn’t brain death. It’s locked in syndrome, and you’ve been medicating her wrong for 2 weeks. The Harvard educated neurologist laughed until Marcus pointed to three symptoms every specialist had missed.
Symptoms he’d memorized from a torn medical textbook he’d been carrying since his sister died from the exact same misdiagnosis 3 years ago. What happened next didn’t just save Sophia’s life. It shattered the arrogance of an entire medical system and proved that knowledge doesn’t require a degree, just the courage to see what others refuse to acknowledge. Marcus hadn’t eaten in 2 days when he made that desperate run through the hospital. But he carried something more valuable than any medical diploma.
The truth that everyone else was too proud to see. This is the story of how a homeless boy with dirt under his fingernails diagnosed what million-dollar doctors couldn’t and why you’ll never look at expertise the same way again. The fluorescent lights of Metropolitan Hospital’s neurological wing hummed with the sterile efficiency of modern medicine. But in room 314, million-doll equipment had become monuments to failure. Dr. Elizabeth Witmore, the hospital’s chief neurologist, and a woman whose personal wealth rivaled small nations, stood before a wall of monitors, displaying the same devastating truth they’d shown for 14 consecutive days.
Sophia Chen, 16 years old, was dying, and nobody knew why. The brain scans remain unchanged. Doctor Whitmore announced to the assembled team of specialists, her voice carrying the kind of authority that came from Harvard Medical School, 30 years of practice and a personal fortune built on medical consulting, complete unresponsiveness to all stimuli, no eye movement, no voluntary muscle control, no indication of higher brain function. The international team she’d personally recruited and funded nodded in solemn agreement. Doctor Hans Miller from Munich whose reputation in neurological trauma was legendary.
Dr. Sarah Kim from Johns Hopkins who’d written the textbook on comeosse states, “Doctor Antoan Dubois from the Saon flown in at Whitmore’s expense because his research on consciousness had revolutionized European medicine. Together they represented over $2 million in consultation fees, decades of combined experience, and the absolute pinnacle of medical education. Together, they had failed completely. The family is becoming difficult, Dr. Whitmore continued, glancing toward the hallway where Sophia’s parents maintained their vigil. They’re asking about alternative treatments, second opinions, experimental procedures.
We need to prepare them for the inevitable conversation about life support. Outside room 314, Maria Chen pressed her ear to the crack in the door, her heart shattering with each clinical word. For 2 weeks, she’d watched her daughter, once vibrant, laughing, preparing for her junior year of high school, lie motionless in a bed surrounded by machines that beeped with mechanical indifference. The doctors spoke in terms Maria didn’t understand, but their expressions told the story clearly enough. They were giving up.
That’s when she saw him. A boy, maybe 12 years old, barefoot and dirty, standing at the far end of the corridor. His clothes were too big, held together with safety pins and hope. His hair was overgrown, his face smudged with the kind of grime that came from sleeping outside. But his eyes, dark, intense, and strangely focused, were fixed on room 314 with an expression Maria had never seen on any of the expensive doctor’s faces. Certainty. The boy approached slowly, clutching something against his chest.

As he came closer, Maria could see it was a book, a medical textbook worn and torn, held together with duct tape and covered in handwritten notes. “Excuse me,” he said softly, his voice carrying a maturity that didn’t match his appearance. “Is that your daughter in there?” Maria blinked, startled. “I Yes. How did you I can help her.” The words hung in the air like a challenge to everything Maria had been told for the past 2 weeks. This child, this homeless boy with no shoes and a textbook that looked like it had been rescued from a dumpster, was claiming he could do what teams of worldrenowned specialists couldn’t.
What did you say? Maria whispered. The boy’s grip tightened on his book. Your daughter, the doctors think she’s brain dead, but she’s not. They’re treating the wrong thing, and every day they continue, they’re making it worse. Before Maria could respond, “Doctor” Whitmore’s voice cut through the hallway like a scalpel. “Security! There’s an unauthorized individual in the ICU.” Two guards appeared almost instantly, their hands already reaching for the boy’s thin shoulders. But Maria Chen, driven by a mother’s desperation, and the first spark of hope she’d felt in 14 days, stepped between them.
“Wait,” she said firmly. “I want to hear what he has to say.” Marcus Williams had been 12 years old for exactly 4 months when he learned that hunger was nothing compared to helplessness. He’d been living on the streets of Chicago for 3 years now, ever since the night that changed everything. And he discovered that while the cold could be endured and the hunger could be ignored, watching someone die when you knew how to save them was a pain that never faded.
His makeshift shelter beneath the Roosevelt Bridge was a carefully constructed fortress of cardboard tarps and scavenged materials. But the real treasure wasn’t the protection from the elements. It was the collection of medical textbooks he’d rescued from dumpsters behind the university. Books that previous students had thrown away after graduation. Books that had become Marcus’ entire world. Gray’s Anatomy, 41st edition. Harrison’s Principles of Internal Medicine. Robins and Kotran pathologic basis of disease. Each book was damaged, missing pages, covered in coffee stains, and highlighting from their previous owners.
But to Marcus, they were perfect. He’d read each one cover to cover multiple times, filling the margins with his own observations and cross references. The other homeless individuals in the area called him little Doc, and they’d learned to trust his advice. When pneumonia threatened the camps during Chicago’s brutal winters, Marcus could identify symptoms early and direct people to the right clinics. When diabetes complications arose among the older residents, he knew which emergency rooms wouldn’t turn them away.
His reputation had spread through the underground network of the forgotten, and people sought him out. But Marcus’s knowledge came from more than textbooks. It came from tragedy. 3 years ago, he’d had a sister, Lily Williams, age 14, the smartest person he’d ever known. She’d been complaining of headaches, difficulty concentrating, occasional episodes where she seemed to zone out completely. Their foster parents had dismissed it as teenage drama. The school nurse had suggested she was attention seeking. Even the emergency room doctor during their one visit had diagnosed stress and sent her home with instructions to get more sleep.
Marcus had known something was wrong. He’d seen the way Lily’s eyes sometimes moved beneath her closed lids during her episodes. The way her fingers would twitch in patterns that seemed too purposeful to be random. He’d tried to tell the adults, but who listens to a 9-year-old boy from the foster system. The night Lily died, officially from what the coroner called sudden unexplained death syndrome, Marcus had stolen into the hospital’s medical library. He’d sat there for hours reading about lockedin syndrome, about partial consciousness, about the thousand ways the brain could be injured without showing obvious external signs.
He’d learned that Lily hadn’t been unconscious during those episodes. She’d been trapped inside her own body, aware but unable to communicate, probably terrified. The diagnosis that could have saved her life was in those textbooks. The treatment was simple, well established, effective, but nobody had thought to look because nobody had taken a 9-year-old’s observations seriously. That night, Marcus had made two decisions. First, he would never again live in a system that had failed his sister so completely. Second, he would learn everything those textbooks contained, so that what happened to Lily would never happen to anyone else if he could help it.
Now standing in the sterile hallway of Metropolitan Hospital, Marcus recognized the symptoms he’d memorized from those late nights reading by flashlight. Sophia Chen wasn’t brain dead. She wasn’t in a coma. She was locked inside her own body, probably terrified, probably aware of every conversation the doctors had about giving up on her. The medical team’s mistake wasn’t just wrong, it was killing her. Every day they continued with their current treatment protocol. They were pushing her deeper into neurological shutdown.
But Marcus knew the pathway back. He’d studied it every night for 3 years, waiting for a chance to save the sister he’d lost. Doctor Elizabeth Whitmore had built her reputation on precision, control, and the absolute certainty that came from superior education and unlimited resources. As she stroed down the hallway toward the disturbance outside room 314, her custom Italian heels clicking against the polished marble floor, she felt the familiar surge of irritation that accompanied any challenge to her authority.
“Chen,” she said, her voice carrying the particular tone she reserved for difficult family members. I understand you’re going through an incredibly difficult time, but allowing unauthorized individuals into our ICU is both against hospital policy and potentially dangerous for your daughter. Maria Chen stood her ground. One protective arm still extended between the security guards and the boy. Dr. Witmore, this child says he knows what’s wrong with Sophia. He says you’re treating the wrong condition. Doctor Whitmore’s laugh was sharp clinical.
Mrs. Chen, I appreciate that desperation can make even the most absurd possibilities seem reasonable, but this child, she gestured dismissively toward Marcus, has no medical training, no credentials, no possible way of understanding your daughter’s condition. My team represents over 60 years of combined neurological experience. We’ve consulted with the finest medical minds in three countries. We’ve run every test known to modern medicine. Marcus stepped forward, his torn textbook clutched against his chest. You ran the wrong tests. The statement hung in the air like a physical slap.
Doctor Whitmore’s eyes narrowed, studying this impossible child who dared to contradict not just her, but the entire foundation of medical hierarchy. Excuse me. Lockedin syndrome presents differently in adolescence, Marcus said, his voice steady despite the tremor in his hands. The neural pathways are still developing, so the classic eye movement responses don’t always appear immediately. You’ve been testing for consciousness using adult parameters, but Sophia’s brain is fighting the condition in ways your protocols don’t account for. Dr. Whitmore felt something she hadn’t experienced in decades.
Uncertainty. Not because she believed this homeless child, but because his words carried a specificity that shouldn’t have been possible. Where exactly did you get this information? Marcus opened his damaged textbook to a page covered in his own handwritten notes. Dr. Elena Vasquez’s research from 2019. She documented 17 cases of atypical lockedin syndrome in patients aged 1417. The diagnostic markers are completely different from adult presentations, but most neurologists don’t know about her work because it was published in a secondary journal.
Dr. Whitmore’s confidence wavered. She did know about Vasquez’s research. It had been controversial, largely dismissed by the mainstream medical community, and yes, it had been published in a journal she didn’t regularly read. Dr. Whitmore, Doctor, Miller interrupted, approaching with the latest test results. The EEG patterns are showing some anomalies we haven’t seen before. There are theta wave fluctuations that don’t fit our current diagnosis. What kind of fluctuations? Marcus asked before Dr. Whitmore could respond. Dr. Mueller blinked, apparently noticing the boy for the first time.
I’m sorry. Who? Show me the patterns. Marcus pressed. If there are theta waves in the 4 to 7 hertz range with occasional gamma spikes above 30 hertz, that’s not brain death. That’s a conscious mind trying to break through neurological barriers. Doctor Whitmore snatched the EEG print out from Dr. Mueller’s hands, her eyes scanning the data. The patterns matched exactly what the boy had described. This is impossible, she whispered. No, Marcus said quietly. It’s just rare. And if you keep treating her for brain death instead of locked in syndrome, those patterns are going to disappear completely.
The medication you’re giving her is suppressing the exact neural activity she needs to recover. For the first time in her 30-year career, Dr. Elizabeth Whitmore found herself facing a possibility that challenged everything she believed about medicine, that this dirty, homeless child might know something she didn’t. And if he was right, her entire team had been slowly killing their patient for 2 weeks. The ICU fell silent except for the mechanical breathing of ventilators and the soft beeping of heart monitors.
Doctor Whitmore stared at the EEG readout in her hands, her mind racing through the implications of what Marcus had just revealed. Around her, the assembled medical team, specialists who had flown in from around the world at her personal expense, waited for her response. “This is absurd,” Dr. Whitmore finally said, but her voice lacked its usual conviction. You’re asking me to completely reconsider a diagnosis based on the observations of a child who has no medical degree, no credentials, no official training whatsoever.
Marcus stepped closer, his bare feet silent against the cold floor. I’m asking you to consider that maybe credentials aren’t the only way to understand medicine. Maybe sometimes the answer comes from paying attention instead of just following protocols. Following protocols, Dr. Whitmore snapped, her authority reasserting itself. Is what separates real medicine from guesswork. It’s what protects patients from from what? Marcus interrupted, his young voice carrying an edge of pain that cut through her professional composure. From people like me, from someone who actually pays attention to what the patient is trying to tell you.
Maria Chen watched the exchange with growing hope and terror. This boy was challenging one of the most powerful doctors in the city, and she could see Dr. Whitmore’s anger building. But she could also see something else. Doubt. Dr. Witmore. Doctor Kim spoke up hesitantly. Perhaps we should at least consider. Consider what? Abandoning 30 years of medical practice because a homeless child read something in a torn textbook? Doctor. Whitmore’s voice rose, echoing off the sterile walls. This is exactly the kind of dangerous thinking that gets patients killed.
Marcus’s grip tightened on his book. The dangerous thinking is what already happened to my sister. The words fell like stones into still water, creating ripples of silence that spread through the gathered medical professionals. Doctor Whitmore’s expression shifted. Some of her anger replaced by curiosity. Your sister, Lily Williams, 14 years old, died 3 years ago from what the coroner called sudden unexplained death syndrome. Marcus’ voice was steady, but his eyes carried the weight of unhealed grief. She had the same symptoms as Sophia, the same EEG patterns, the same theta wave fluctuations.
And the doctors did the same thing you’re doing. They followed protocols instead of listening. Dr. Whitmore felt something cold settle in her stomach. What are you suggesting? I’m suggesting that maybe if one doctor had taken 5 minutes to consider that a 14-year-old girl’s brain might work differently than an adults, my sister would still be alive. Marcus looked directly at Dr. Witmore, his young face carrying the weight of years spent studying every detail of his sister’s case. and I’m suggesting that if you don’t stop the current medication protocol and start treating Sophia for lockedin syndrome, you’re going to kill her the same way they killed Lily.
The accusation hung in the air like a physical presence. Dr. Whitmore felt the eyes of her entire team on her. Felt the weight of her reputation, her career, her self-image as a healer, all balanced on a knife’s edge. You’re asking me to risk my patients life on the medical opinion of a 12-year-old homeless boy? No, Marcus said quietly. I’m asking you to risk your pride to save her life. Doctor Whitmore stared at him for a long moment, then at the EEG readout in her hands.
Then at room 314, where Sophia Chen lay connected to machines that might be slowly killing her. “If I give you 5 minutes to examine her,” she said slowly. “And if your assessment proves incorrect, I’ll have you arrested for interfering with medical treatment. ” Marcus nodded without hesitation. And if I’m right, doctor Whitmore’s jaw tightened. If you’re right, then everything I’ve believed about medicine for 30 years needs to be reconsidered. Deal. The news spread through Metropolitan Hospitals corridors like electricity through water.
Nurses paused in their rounds. Orderly whispered in supply closets, and residents gathered in small clusters, all discussing the impossible scene unfolding in the neurological wing. A homeless child was about to examine a patient that the most expensive medical team in the city had given up on. Nurse Patricia Rodriguez, who had worked the ICU for 15 years, stood outside room 314 with her arms crossed, watching Dr. Whitmore lead the boy toward Sophia’s bedside. “This is the most ridiculous thing I’ve ever seen,” she muttered to her colleague.
“That child probably doesn’t even know what a stethoscope is for.” But even as she spoke, Patricia remembered something that had been nagging at her for days. During her night shifts, when the room was quiet and the family had gone home to rest, she’d noticed tiny movements from Sophia. Nothing dramatic, nothing that would show up on the monitors, but small things. A slight change in breathing pattern when voices rose in the hallway, a barely perceptible shift in facial expression when certain songs played on the radio.
She had mentioned it to Dr. Whitmore once, but the doctor had dismissed it as wishful thinking. Postcomos reflexes, she’d called them, meaningless neural static. Now, watching Marcus approached Sophia’s bed with a reverence that none of the milliondoll specialists had shown, Patricia found herself wondering if those movements had been meaningless after all. In the family waiting area, word had reached the other families keeping vigil. Tom Bradley, whose wife was recovering from brain surgery two rooms down, shook his head in disbelief.
They’re letting a street kid examine patients now. What’s next? Having janitors perform surgery. But Maria Chen’s sister, who had arrived from Phoenix that morning, watched through the window with growing interest. “Look at him,” she whispered to Maria. “Look at how he’s moving around her bed. He’s not just looking at the machines. He’s looking at her.” It was true. While Dr. Whitmore and her team had spent two weeks focused on monitors, readouts, and test results. Marcus was studying Sophia herself.
He moved slowly around the bed, observing her from different angles, his eyes tracking tiny details that escaped clinical observation. In the hospital’s administrative offices, news of the unusual situation had reached Dr. James Morrison, Metropolitan’s Chief of Staff. He stood at his window overlooking the ICU wing, phone in hand, debating whether to call security to end this medical circus before it damaged the hospital’s reputation. “Sir,” his assistant said hesitantly. “Dr. Whitmore’s team represents significant financial investment if this child somehow discredits their work.” Dr.
Morrison nodded grimly. Metropolitan Hospital’s reputation was built on attracting the world’s best medical minds. They charged premium rates because they delivered premium results. A homeless child succeeding where international specialists had failed would raise uncomfortable questions about the value of expensive medical care. But even as he considered ending the examination, doctor Morrison found himself curious. In 30 years of hospital administration, he’d seen medical miracles, but he’d also seen medical arrogance. Sometimes the most expensive diagnosis wasn’t the correct one.
Back in room 314, the tension was palpable. Marcus knelt beside Sophia’s bed, his torn textbook opened to a page filled with his handwritten notes. He began speaking in a low voice, not to the assembled doctors, but directly to Sophia. Hi, Sophia. My name is Marcus. I know you can hear me even if nobody else believes it. I know you’re trapped in there, and I know you’re scared, but I want you to know that someone finally understands what’s happening to you.
Dr. Whitmore started to interrupt. Talking to comeosse patients was considered therapeutic but ultimately meaningless. But something stopped her. Sophia’s heart rate monitor showed a slight increase in rhythm. Marcus continued. I’m going to ask you to do something very simple. If you can hear me if you understand what I’m saying, I want you to try to blink twice. Don’t worry if it doesn’t work perfectly. Your brain is fighting through a lot of interference right now. The room fell silent.
14 pairs of medical professional eyes focused on Sophia’s closed eyelids. And then slowly, deliberately, Sophia Chen blinked twice. The two deliberate blinks sent shock waves through room 314. Dr. Whitmore stumbled backward, her face pale, while Dr. Mueller grabbed the nearest chair for support. The monitors showed clear increases in Sophia’s heart rate and blood pressure. Responses that shouldn’t have been possible in a brain deadad patient. “That was that was voluntary movement, doctor,” Kim whispered, her voice barely audible above the mechanical hum of the life support equipment.
Marcus remained calm, his hand gently resting on Sophia’s arm. “Sophia, you’re doing great. Can you try to squeeze my hand?” Just a little pressure. The faintest squeeze came immediately, so slight that only Marcus felt it, but it was enough. “She’s conscious,” he said simply, turning to face the stunned medical team. “She’s been conscious this entire time, trapped inside a body that stopped responding normally. Every conversation you’ve had about ending life support, every decision you’ve made without her input, she’s heard all of it.” Maria Chen collapsed into a chair, tears streaming down her face.
For 2 weeks, she’d talked to her daughter about everything. School, friends, the weather, her fears about losing her, never knowing that Sophia had heard every word. Doctor Whitmore found her voice, though it came out as barely more than a whisper. “How did you know? How could you possibly have identified what we missed?” Marcus’s expression grew distant, and for a moment the professional composure he’d maintained cracked, revealing the griefstricken 12-year-old beneath because I watched my sister die from the same thing.
He opened his worn textbook to a page near the back where a photograph was taped to the margin. The picture showed a young girl with Marcus’s eyes and smile, her arm around a smaller boy who was unmistakably Marcus at age nine. Lily Williams, she started having episodes when she was 13. moments where she’d just stop. Her eyes would go blank, her body would go limp, but something about it didn’t seem like regular unconsciousness. During those episodes, I noticed her eyes would move in patterns, like she was trying to communicate.
Marcus’ voice grew steadier as he continued, drawn back into memories he’d relived countless times. The doctors said it was stress, maybe some kind of teenage hysteria. But even when the episodes got longer, even when she stopped responding to her name, they kept saying it was psychological. What happened to her? Doctor, Whitmore asked, though her medical instincts already suggested the terrible answer. She had an episode that lasted 3 days. The doctors said she was catatonic, that it was a severe psychological break.
They put her on sedatives to calm her system. Marcus’s hands trembled slightly as he turned the page in his textbook, revealing pages of meticulous notes in a child’s handwriting. Those sedatives suppressed the exact neural pathways she needed to break through the lockedin state. Instead of helping her communicate, they pushed her deeper into neurological shutdown. The room remained silent except for the soft beeping of Sophia’s monitors. monitors that were now showing patterns of awareness instead of the flat lines of brain death.
After Lily died, I stole every medical textbook I could find. I read everything about consciousness, about comas, about locked in syndrome. I learned that the doctors had been wrong about everything. Marcus looked up at Dr. Whitmore with eyes that carried far too much knowledge for someone his age. Lily wasn’t mentally ill. She wasn’t catatonic. She had a typical lockedin syndrome, probably caused by a viral infection that created inflammation in her brain stem. And the treatment, Dr. Whitmore asked, though she suspected she already knew, simple anti-inflammatory medication to reduce the brain stem swelling combined with specific neural stimulation exercises to reestablish communication pathways.
The success rate is over 90% if caught early. Marcus’ voice carried the weight of 3 years worth of studying the cure that could have saved his sister. The treatment protocol has been established for 15 years. It was in every textbook, but nobody thought to look because nobody took a 9-year-old’s observations seriously, a doctor. Whitmore stared at Sophia, whose breathing had become more regular, whose facial expressions seemed more peaceful since Marcus had begun talking to her. You’re saying we’ve been killing her slowly for 2 weeks?
Yes, Marcus said simply, “But she’s still savable. The question is whether you’re willing to admit you were wrong.” Dr. Whitmore’s world tilted on its axis. For 30 years, she had been the voice of medical authority, the final word on complex diagnosis, the doctor other doctors consulted when cases seemed hopeless. Her reputation had been built on precision, confidence, and an unwavering belief in the superiority of institutional medical knowledge. Now, a homeless 12-year-old was suggesting that everything she’d believed about this case was not just wrong, but lethally wrong.
“This is impossible,” she said, but her voice lacked conviction. You’re asking me to believe that a child with no formal medical training has identified a condition that escaped the notice of specialists from Harvard, Johns Hopkins, and the Saon. Marcus looked at her steadily. I’m asking you to believe that sometimes experience matters more than credentials. Dr. Whitmore felt her authority slipping away like sand through her fingers. Around the room, she could see doubt creeping into the expressions of her carefully assembled team.
Dr. Miller was reviewing his own notes with new uncertainty. Dr. Kim was studying Sophia’s face with fresh attention. Doctor Dubois was quietly checking the medication protocols they’d been following. Dr. Whitmore. Dr. Kim spoke hesitantly. Perhaps we should consider running some additional tests. If there’s even a possibility, a possibility based on what? Dr. Whitmore snapped, her professional composure cracking. the opinion of a street child who learned medicine from damaged textbooks. Do you understand what you’re suggesting? That our entire diagnostic process, our years of education, our internationally recognized expertise, all of it is worthless compared to the observations of a homeless boy.
But even as she spoke, Dr. Whitmore was remembering inconsistencies she’d dismissed over the past 2 weeks. Sophia’s EEG patterns that didn’t quite fit standard brain death criteria. the way her vital signs sometimes fluctuated without apparent cause. The nursing staff’s reports of subtle movements that the monitors hadn’t detected. Marcus stepped closer to Sophia’s bed, his voice calm despite the tension filling the room. Sophia, I know this is scary, but these doctors need to understand that you’re still in there.
Can you try to move your right index finger? Just a tiny movement. Doctor Whitmore was about to protest that voluntary movement was impossible in Sophia’s condition when she saw it. The faintest twitch of Sophia’s right index finger. “Did you see that?” Maria Chen gasped, pointing at her daughter’s hand. “Muscle spasm,” Dr. Whitmore said quickly, but her voice was shaking. “Random neural firing. It doesn’t indicate consciousness.” “Sophia,” Marcus continued, ignoring Dr. Whitmore’s explanation. Can you do it again?
Move your finger one more time to show them you understand. The finger moved again, this time more deliberately. Dr. Meler stepped forward, his face pale. Elizabeth, that’s not random neural firing. That’s responsive movement. Dr. Whitmore felt panic rising in her chest. If Marcus was right, if Sophia had been conscious throughout her treatment, then every decision the medical team had made was not just wrong, but potentially criminal. The medications they’d administered, the procedures they’d performed, the conversations they’d had about ending life support, all of it had been done to a conscious, aware patient.
“This proves nothing,” she said desperately. “Patients in vegetative states can exhibit responsive movements. It doesn’t indicate higher brain function. ” Marcus opened his textbook to another marked page. “Dr. Whitmore, would you be willing to test her cognitive function?” “What do you mean?” Ask her mathematical questions. Questions that require thinking, not just reflexive responses. If she can answer by blinking, once for no, twice for yes, it will prove she’s not only conscious, but cognitively intact. Dr. Whitmore found herself trapped.
If she refused to test Sophia’s cognitive function, she would appear to be avoiding evidence that contradicted her diagnosis. If she agreed to test and Sophia demonstrated awareness, her entire career would be called into question. But if she agreed to test and Sophia failed to respond, she could discredit Marcus completely and restore her medical authority. “Fine,” she said, her voice tight with tension. “But when this test fails to show cognitive function, I want this child removed from my hospital immediately,” Marcus nodded.
“And if the test shows that Sophia is cognitively intact, Dr. Whitmore met his gaze, her jaw set with determination. Then I’ll implement whatever treatment protocol you recommend. The ICU fell into a silence so complete that the mechanical breathing of ventilators seemed unnaturally loud. Doctor Witmore approached Sophia’s bedside, her hands trembling slightly as she prepared to conduct a test that could either vindicate her medical judgment or destroy everything she’d built her career upon. Sophia, Dr. Whitmore said, her voice formal and clinical.
If you can hear and understand me, I’m going to ask you some questions. Blink once for no, twice for yes. Do you understand? Two clear, deliberate blinks. Maria Chen gripped her sister’s hand so tightly that her knuckles went white. Around the room, medical professionals who had spent decades studying consciousness found themselves witnessing something that challenged every assumption they’d made about Sophia’s condition. Sophia, doctor, Whitmore continued, her voice growing more strained. Are you 16 years old? Two blinks.
Are you in a hospital? Two blinks. Dr. Whitmore’s hands were shaking now. These responses could still be coincidental, reflexive, meaningless. But the pattern was becoming impossible to ignore. Sophia, I’m going to ask you a mathematical question. What is 7 + 5? If the answer is 12, blink twice. If it’s not 12, blink once. The pause seemed to last forever. Then, clearly and deliberately, Sophia blinked twice. Dr. Kim let out a small gasp. Doctor Mer stepped closer to the bed, his face a mask of disbelief.
Dr. Dubois was frantically taking notes, documenting responses that shouldn’t have been possible. One more question, doctor, Whitmore said, her voice barely above a whisper. Sophia, what month were you born? If it was June, blink twice. if it was any other month. Blink once. Marcus watched Dr. Witmore’s face as she asked the question, recognizing the tactical nature of it. She was testing not just Sophia’s cognitive function, but whether the responses were truly voluntary or somehow being prompted. Sophia blinked once.
“She was born in September,” Maria Chen whispered. “Her birthday is September 15th.” Dr. Whitmore staggered backward, her face drained of color. The implications were staggering. Not only was Sophia conscious, but she was cognitively intact, aware of her surroundings, and had been listening to every conversation about her condition for the past 2 weeks. Marcus stepped forward, his voice gentle but firm. Dr. Whitmore, Sophia has been trapped inside her own body while your team discussed ending her life support.
She’s heard every word about how hopeless her case is, how expensive her care has become, how it might be more humane to let her die. The words hit Dr. Whitmore like physical blows. In her 30-year career, she had never faced the possibility that she had been torturing a conscious patient with her clinical discussions about their hopeless prognosis. Sophia, Marcus continued, can you forgive these doctors for not understanding your condition? Blink twice for yes, once for no. The room held its collective breath.
After everything Sophia had endured, after 2 weeks of being treated as an unconscious object rather than a person, her response would be the ultimate test of grace and humanity. Sophia blinked twice. Doctor Fitmore broke down completely, tears streaming down her face as the full weight of her mistake became clear. She had built her career on the assumption that medical expertise was synonymous with expensive education and institutional authority. But a homeless child with a torn textbook had demonstrated more diagnostic insight than her entire international team.
“What’s the treatment?” she whispered, her voice broken. Marcus opened his textbook to a detailed treatment protocol he’d copied from multiple sources. anti-inflammatory medication to reduce brain stem swelling, specific neural stimulation exercises to reestablish communication pathways, and most importantly, immediate discontinuation of the sedatives that have been suppressing her neural recovery. The transformation in room 314 was immediate and profound. Within minutes of Marcus explaining the treatment protocol, Dr. Whitmore had ordered the nursing staff to discontinue the seditive medications that had been keeping Sophia in artificial neurological suppression.
As the drugs began to clear from her system, the changes became visible on every monitor in the room. Her EEG patterns are normalizing. Doctor Kim announced, her voice filled with wonder as she watched brainwave activity that had been flat for 2 weeks suddenly show signs of consciousness. Theta waves are stabilizing and we’re seeing alpha wave patterns consistent with aware but relaxed consciousness. Marcus knelt beside Sophia’s bed, his voice gentle but urgent. Sophia, the medicine that was making it hard for your brain to work is being stopped.
You might start feeling more aware, more able to move. Don’t be scared if sensations start coming back. That’s your nervous system healing. Dr. Whitmore watched in stunned silence as Marcus demonstrated the neural stimulation exercises he’d learned from his textbook research. Simple techniques, gentle pressure on specific points along Sophia’s arms and legs, exercises designed to reactivate dormant neural pathways, movements that encouraged her brain to rebuild connections that had been disrupted by inflammation. “Where did you learn these techniques?” Dr.
Miller asked. His earlier skepticism replaced by genuine professional curiosity. Marcus looked up from his work with Sophia. Doctor Elena Vasquez’s research included detailed rehabilitation protocols. She found that lockedin syndrome patients recover faster when treatment begins immediately. But most hospitals don’t know about her methods because her work was published in smaller journals. Why smaller journals? Doctor Dubois asked. because she was treating homeless patients in free clinics,” Marcus replied simply. The medical establishment didn’t consider her research relevant to real hospital populations.
The irony wasn’t lost on anyone in the room. The research that could save Sophia had been dismissed by mainstream medicine because it focused on patients exactly like Marcus, people without insurance, without social status, without the kind of institutional backing that gave medical research credibility. As Marcus continued the neural stimulation exercises, something remarkable began to happen. Sophia’s breathing, which had been mechanically regulated for 2 weeks, started to show natural variation. Her heart rate stabilized at patterns consistent with natural sleep rather than medically induced unconsciousness.
Sophia, Marcus said softly, I want you to try something for me. Try to wiggle your toes. Don’t worry if it doesn’t work perfectly. Your brain is just remembering how to control your body. Maria Chen watched her daughter’s feet with desperate intensity. For several seconds, nothing happened. Then slowly, almost imperceptibly, Sophia’s right big toe moved. “Oh my god,” Maria whispered, her hands covering her mouth. “She moved her toe. She actually moved her toe. ” “Doctor Whitmore felt something she hadn’t experienced since her early days as a medical student.
the pure wonder of witnessing healing that seemed miraculous but was actually the result of proper diagnosis and treatment. For 2 weeks, she had been administering medication that suppressed the exact neural activity Sophia needed to recover. Marcus had identified the problem and provided the solution within 15 minutes of examining her. The anti-inflammatory medication should be administered intravenously, Marcus continued, consulting his notes. Methyl predniscolone 30 mg per kilogram of body weight followed by a maintenance dose for 7 days.
The brain stem inflammation should begin reducing within 6 to 8 hours. Dr. Whitmore found herself taking medical orders from a 12-year-old homeless boy and for the first time in her career. It felt completely appropriate. Marcus understood Sophia’s condition better than anyone else in the room because he had lived with the consequences of medical ignorance. His sister’s death had given him a level of knowledge that no medical school could provide. “Marcus,” Dr. Whitmore said quietly. “What made you come to this hospital tonight?” Marcus looked up from Sophia, his young face serious.
“I’ve been checking hospitals around the city for 3 years, looking for cases like Lily’s. When I heard about Sophia on the news, a teenage girl in an unexplained coma, I knew I had to try. You’ve been doing this for 3 years. Every night, Marcus confirmed, looking for patients the doctors have given up on. Cases where the symptoms match what I learned studying Lily’s condition. Doctor Whitmore realized she was witnessing something unprecedented. A 12-year-old boy had been conducting his own medical practice on the streets of Chicago, using knowledge gained from grief and determination to save lives that the official medical system had written off.
And he had been succeeding where they had failed. Word of Sophia’s improvement spread through Metropolitan Hospital like wildfire. Within hours, medical staff from other departments began finding excuses to walk past room 314, hoping to catch a glimpse of the homeless boy who had accomplished what a million dollar medical team couldn’t. Doctor James Morrison, the hospital’s chief of staff, arrived at 3:00 a.m. to witness the situation firsthand. He found Dr. Whitmore sitting beside Sophia’s bed, carefully monitoring the neural stimulation exercises that Marcus had taught her to perform.
Elizabeth, Dr. Morrison said quietly. Is it true? Did a homeless child really diagnose lockedin syndrome when your entire team missed it? Dr. Whitmore looked up, her face showing the exhaustion and humility of someone whose fundamental beliefs had been shattered. Not just diagnosed it, Jim, he’s treating it and it’s working. On the monitors, Sophia’s brain activity continued to improve. The theta wave patterns that had been chaotic for 2 weeks were stabilizing into coherent rhythms. Her muscle responses were becoming more coordinated.
Most remarkably, she had begun to exhibit REM sleep patterns for the first time since her hospitalization. “Where is the boy now?” Dr. Morrison asked. “In the family lounge,” Dr. Whitmore replied. He’s been awake for 20 hours straight monitoring Sophia’s progress and adjusting the treatment protocol based on her responses. Doctor Morrison found Marcus in the small family lounge, curled up in a chair with his torn medical textbook open on his lap. Even in sleep, the boy’s hand rested protectively on the book that had become his most precious possession.
“Excuse me,” Dr. Morrison said gently, not wanting to startle him. Marcus woke immediately, his eyes alert despite his exhaustion. Is Sophia okay? Do the monitors show continued improvement? Doctor Morrison was struck by the boy’s immediate concern for his patient, a level of medical dedication that he rarely saw even in experienced physicians. She’s doing well. Her neural responses are continuing to strengthen. Good, Marcus said, relief evident in his voice. The anti-inflammatory medication should reach peak effectiveness within the next few hours.
Her communication abilities should improve significantly by morning. Doctor Morrison sat down across from Marcus, studying this remarkable child who had challenged everything Metropolitan Hospital believed about medical expertise. Marcus, I need to ask you something. How many other cases like this have you encountered? Marcus was quiet for a moment, then opened his textbook to a section near the back. The pages were covered with handwritten notes documenting dozens of cases, names, dates, symptoms, hospitals, outcomes. 17 patients in the past 3 years, Marcus said simply.
12 recoveries, three partial recoveries, two cases where I arrived too late. Dr. Morrison felt his breath catch. You’re telling me that you’ve been successfully treating patients across the city without anyone knowing? Not treating, Marcus corrected. Diagnosing. Once I identify the correct condition, I try to get the information to the medical teams. Sometimes they listen, sometimes they don’t. And when they don’t listen, Marcus’s expression grew sad. People die from treatable conditions because doctors are too proud to consider that their diagnosis might be wrong.
Dr. Morrison realized he was facing a medical phenomenon unlike anything he’d encountered in 30 years of hospital administration. This homeless child had been conducting a shadow medical practice, identifying diagnostic errors, and correcting them when possible, all while living on the streets and surviving on charity. Marcus, what would you say if I told you that this hospital wants to offer you a formal position, medical consultant with full access to our facilities and resources? Marcus looked surprised. You want to hire me?
I want to learn from you, Dr. Morrison said honestly. You’ve demonstrated diagnostic abilities that our most expensive specialists lack. You understand medicine in ways that medical school doesn’t teach. Marcus considered this for a moment, then shook his head. I appreciate the offer, but there are too many patients in other hospitals who need help. I can’t stay in one place when there are people dying from mistakes that could be prevented. Dr. Morrison found himself face to face with a level of medical dedication that put his entire professional staff to shame.
This 12-year-old boy had turned his personal tragedy into a mission to save lives, and he was unwilling to compromise that mission for comfort or security. “Then what would you say to a partnership?” Dr. Morrison asked. “Metropolitan Hospital could sponsor your work citywide. Give you resources, credentials, support.” For the first time since Dr. Morrison had met him, Marcus smiled. “Now that,” he said, “sounds like something Lily would have wanted. The confrontation that had been building for hours finally erupted at 6:00 a.m.
when Dr. Whitmore could no longer contain her professional shame and personal revelation. She found Marcus in the hospital cafeteria, sitting alone at a corner table with a cup of coffee that a sympathetic nurse had brought him and his everpresent medical textbook. “I need to talk to you, doctor,” Whitmore said, sliding into the seat across from him. Her usually perfect appearance was disheveled, her designer clothing wrinkled from the long night, her carefully styled hair falling loose around her face.
“Marcus looked up from his textbook, his young eyes meeting hers with a directness that she found both uncomfortable and necessary.” “I’ve been thinking about what you said,” Dr. Whitmore continued, her voice tight with emotion. “About credentials versus knowledge, about pride versus patient care, and I need to understand something. What’s that? How does a 12-year-old homeless boy know more about medicine than doctors who spent decades studying it? Marcus was quiet for a moment, considering his response. Maybe because I study medicine to save lives, not to make money or build reputations.
The words hit Dr. Witmore like a physical blow because she recognized the truth in them. When had her practice of medicine become more about maintaining her status than healing patients? When had she stopped seeing patients as people and started seeing them as cases to be solved or problems to be managed? You’re saying I became a doctor for the wrong reasons? I’m saying maybe you forgot the right reasons, Marcus replied gently. When I read medical textbooks, every page reminds me of Lily.
Every symptom description makes me think about patients who might be suffering from conditions that doctors miss. When you read medical literature, what do you think about? Doctor Whitmore realized with crushing clarity that she thought about publications, prestige, professional advancement. She thought about complex cases that would enhance her reputation, and lucrative consultations that would increase her wealth. She couldn’t remember the last time she had read medical research simply because it might help her understand a patient’s suffering. My sister died because doctors like you couldn’t imagine that a 9-year-old might notice something important.
Marcus continued, his voice steady but carrying deep pain. They dismissed my observations because I didn’t have credentials. They ignored evidence because it came from someone they considered unqualified to have opinions about medicine. And now you’re doing the same thing to me that they did to you,” Dr. Whitmore said quietly, judging my knowledge based on my credentials instead of my results. Marcus shook his head. No, Dr. Whitmore. I’m judging your knowledge based on your results. For two weeks, your credentials led you to slowly kill a conscious patient.
My lack of credentials led me to save her life in one night. The statement hung between them like a chasm that couldn’t be crossed with explanations or justifications. Doctor Whitmore had spent 30 years building a career on the assumption that medical education was the only path to medical knowledge, that institutional authority was synonymous with correctness, that expensive specialists were inherently superior to less credentialed practitioners. Marcus had proven all of those assumptions catastrophically wrong. What do you want from me?
Dr. Whitmore asked finally. I want you to remember why you became a doctor, Marcus replied. I want you to look at patients instead of just looking at test results. I want you to listen to families even when they’re not medical professionals. And I want you to consider that sometimes the most important medical insights come from people who understand suffering, not just people who understand systems. Doctor Whitmore felt tears building in her eyes as she realized that this homeless child was offering her something she hadn’t experienced in decades.
the opportunity to remember what it meant to be a healer rather than just a medical technician. How do I do that? She whispered. How do I change everything I’ve believed about medicine? Marcus reached across the table and gently touched her hand. You start by admitting that credentials don’t make you a better doctor. Caring does, and then you prove it by using your position to help patients that other doctors have given up on. Doctor Witmore looked into the eyes of this remarkable child and saw not just wisdom beyond his years, but a path toward redemption that she had never imagined possible.
“Will you teach me ?” she asked. Marcus smiled for the second time since she’d met him. “I’ll learn with you.” At 7:30 a.m., exactly 18 hours after Marcus had first burst through the ICU doors, Sophia Chen opened her eyes. The moment was witnessed by her parents, who had maintained their vigil through the night, by Marcus, who had been monitoring her neural responses every 15 minutes, and by Dr. Witmore, who had been documenting the unprecedented recovery in meticulous detail.
Sophia, Maria Chen whispered, her voice barely audible in the quiet room. Baby, can you see me? Sophia’s eyes moved slowly, tracking her mother’s voice until their gazes met. Then, with effort that was visible but determined, she whispered her first word in two weeks. Mom. The sound of her daughter’s voice broke Maria Chen completely. Two weeks of silent bedside vigils, of medical consultations that offered no hope, of preparing herself for the possibility of losing her child. All of it dissolved in the miracle of that single word.
I’m here, sweetheart,” Maria sobbed, taking Sophia’s hand and feeling the gentle pressure of her daughter’s responding squeeze. “I’m right here.” Marcus stepped closer to the bed, his medical textbook clutched against his chest. “Sophia, do you remember me? I’m Marcus. I’ve been helping your doctors understand your condition. ” Sophia’s eyes found Marcus, and her lips curved into the faintest smile. You saved me,” she whispered, her voice growing slightly stronger with each word. “No,” Marcus said gently. “I just helped everyone understand that you were still in there fighting to come back.” Dr.
Whitmore watched this exchange with emotions she couldn’t fully process. For 2 weeks, she had been treating Sophia as a medical case, a complex diagnostic challenge to be solved with expensive tests and international consultations. Marcus had treated her as a person, someone trapped and scared who needed to be heard and understood. Sophia, Dr. Whitmore said, stepping forward. I owe you an apology. My team and I misunderstood your condition, and our treatment was making you worse instead of better.
I’m deeply sorry. Sophia looked at Dr. Whitmore with eyes that held no anger, only relief. I heard everything, she whispered. All the conversations about giving up. I wanted to tell you I was still here. The full weight of the medical team’s mistake became devastatingly clear. Sophia had been conscious throughout her entire hospitalization, listening to clinical discussions about her hopeless prognosis, hearing debates about the cost effectiveness of her care, being present for conversations about end of life decisions.
She had been trapped inside her own body while medical professionals made decisions about her future without recognizing that she was aware enough to have opinions about those decisions. How do you feel now? Marcus asked, his voice carrying the professional concern of someone monitoring a patients recovery. Tired, Sophia admitted, but clear like fog is lifting from my brain. My body feels heavy, but I can feel everything now. Before it was like being underwater, hearing sounds but not being able to respond.
Marcus nodded, consulting his notes. That’s exactly what lockedin syndrome feels like. Your brain was working normally, but the inflammation in your brain stem was preventing the signals from reaching your muscles properly. Doctor Whitmore realized she was witnessing something unprecedented in her medical career. A patient who could describe the subjective experience of a condition that most doctors only understood clinically. Sophia’s insights could revolutionize how lockedin syndrome was diagnosed and treated. Sophia, Dr. Dr. Whitmore said carefully, “Would you be willing to help us understand your experience?
What you felt during the past 2 weeks could help other patients in similar situations?” Sophia looked at Marcus, who nodded encouragingly. “If it helps other people not go through what I went through,” she said. “I want to help.” Marcus smiled, recognizing in Sophia the same determination to prevent suffering that had driven his own medical education. I think he said quietly that’s exactly what Lily would have wanted too. For the first time since her recovery began, Sophia asked the question that would change everything.
Who’s Lily? And Marcus began to tell the story that had brought them all together. The story of a sister whose death had taught her brother that sometimes the most important medical knowledge comes not from textbooks, but from love. Within hours of Sophia’s awakening, Metropolitan Hospital became the center of a medical storm that would reshape how the institution viewed diagnostic expertise. Doctor James Morrison found himself fielding calls from medical journals, news outlets, and hospital administrators from around the country, all wanting to understand how a homeless child had succeeded where internationally renowned specialists had failed.
Morrison, the reporter from the Chicago Tribune, pressed during his third interview of the morning, “What does this say about the state of modern medicine when a 12-year-old with no formal training can outdose Harvard educated physicians?” The question struck at the heart of what Dr. Morrison knew would become a national conversation about medical authority, institutional credibility, and the relationship between expensive health care and effective healthcare. What it says, Dr. Dr. Morrison replied carefully is that medicine is more complex than any single educational path can address.
Marcus Williams brought perspectives to diagnosis that our traditional medical training hadn’t prepared us for. But even as he spoke the diplomatic words, Dr. Morrison knew the implications were far more dramatic. Metropolitan Hospital had charged the Chen family over $400,000 for 2 weeks of incorrect treatment that had actually made their daughter worse. Meanwhile, a homeless boy with a torn textbook had provided the correct diagnosis and treatment protocol within hours, asking for nothing in return. In room 314, the medical team that had been so confident in their expertise was grappling with a professional identity crisis.
Doctor Müller stood by the window, staring out at the city skyline, trying to process how his 20 years of neurological experience had led him so completely astray. How did we miss it? He asked. Doctor Kim, who was reviewing Marcus’ treatment notes with growing amazement. The symptoms were there. The EEG patterns were actually consistent with lockedin syndrome if we’d been looking for it. We weren’t looking for it because we didn’t believe it was possible, Dr. Kim replied. We saw a teenager in an unresponsive state and immediately assumed brain death.
We never considered that her brain might be functioning normally but unable to communicate through conventional pathways. Dr. Dubois was having a more personal crisis. He had flown in from Paris specifically because of Dr. Whitmore’s reputation and the intellectual challenge of an unsolvable case. Now he was faced with the reality that the case had been solvable from the beginning if anyone had been willing to consider non-traditional diagnostic approaches. I keep thinking, he said to no one in particular, about all the times I’ve dismissed family members who insisted their loved ones were still in there.
How many conscious patients have I treated as unconscious because I was too proud to consider alternative possibilities? The nursing staff was experiencing their own revelation. Patricia Rodriguez, the ICU nurse who had noticed Sophia’s subtle responses during night shifts, felt vindicated but also frustrated. I told doctor quit more about the movements I was seeing, she said to her colleague during their break. But when a homeless kid says the same thing, suddenly it’s worth investigating. What does that say about whose observations we value?
Marcus, meanwhile, was experiencing something he hadn’t felt since before Lily’s death, hoped that the medical system might actually change. As he sat with Sophia, helping her practice the motor control exercises that would speed her recovery, he allowed himself to imagine a world where doctors listened to patients and families instead of just consulting with other doctors. Marcus, Sophia said during one of their sessions, “What you did for me, do you think it could help other people?” “I hope so,” Marcus replied.
But it’s going to require doctors who are willing to admit they don’t know everything and patients who are brave enough to share their experiences even when medical professionals don’t want to hear them. Sophia looked at him with the clarity of someone who had experienced both the worst and best of medical care within the span of a single day. Then let’s make sure that happens. outside room 314. Doctor Whitmore was on the phone with the hospital’s legal department discussing how to address the financial and ethical implications of 2 weeks of incorrect treatment.
But more importantly, she was beginning to understand that her medical career had reached a turning point that would define not just her future practice, but her fundamental identity as a physician. The question was whether she had the courage to embrace the transformation that Marcus had made possible. The reckoning came swiftly and decisively. By 2 p.m., less than 24 hours after Marcus had first appeared in the ICU, Metropolitan Hospital’s board of directors had convened an emergency meeting to address what hospital attorney Patricia Walsh was calling the most significant diagnostic failure in the institution’s history.
Dr. Elizabeth Whitmore sat alone in the boardroom’s waiting area, her 30-year career hanging in the balance. Through the glass doors, she could hear fragments of heated discussion about liability, malpractice exposure, and institutional credibility. Her name was mentioned repeatedly, not with the respect she had grown accustomed to, but with the kind of clinical detachment typically reserved for discussing problematic cases. Doctor Whitmore, the board chairman, Robert Chen, ironically no relation to Sophia, called her into the meeting. We need to understand exactly what happened with the Chen case.
Doctor Whitmore faced 12 board members, colleagues she had worked with for years, now looking at her with expressions ranging from disappointment to barely contained anger. She realized that this was how patients must feel when medical professionals discussed their cases, reduced to a problem to be managed rather than treated as a person deserving dignity. The facts are straightforward. She began her voice steady despite her inner turmoil. My team and I misdiagnosed Sophia Chen’s condition, leading to two weeks of treatment that suppressed rather than supported her recovery.
“A 12-year-old homeless boy identified the correct diagnosis within minutes of examining her. ” “And the financial implications?” asked the hospital’s chief financial officer. We charged the family $487,000 for treatment that was not only ineffective but actively harmful, Dr. Whitmore admitted. Marcus Williams provided the correct diagnosis and treatment protocol at no cost. The room fell silent as the board members absorbed the magnitude of the institutional failure. Metropolitan Hospitals reputation was built on providing premium medical care justified by premium prices.
The Chen case suggested that their most expensive specialists were not just inferior to a homeless child’s diagnostic abilities, but potentially dangerous. Doctor Whitmore, Chairman Chen said finally, “Given the severity of this diagnostic failure and its implications for patient safety, the board has decided to request your resignation effective immediately. ” Doctor Whitmore had expected this outcome, but hearing it spoken aloud still felt like a physical blow. I understand, she said quietly. But before I leave, I want to make a recommendation.
What kind of recommendation? Hire Marcus Williams as a diagnostic consultant. Give him credentials, resources, and authority to review cases where traditional approaches have failed. His insights could revolutionize how this hospital practices medicine. Board member Dr. Sarah Thompson leaned forward. “You’re suggesting we hire a homeless child to supervise our medical staff. I’m suggesting you hire someone who understands medicine in ways that medical school doesn’t teach,” Dr. Whitmore replied. Marcus has successfully diagnosed 17 cases that other doctors missed.
“His methodology could save lives and prevent exactly the kind of institutional failure that we’re dealing with today,” Chairman Chen made notes on his tablet. And what about the financial implications of the Chen case? Doctor Whitmore took a deep breath before making the most important recommendation of her career. Refund the entire treatment cost. Publicly acknowledge our diagnostic failure. Use this case as an opportunity to demonstrate that Metropolitan Hospital values patient care over institutional pride. That would cost nearly half a million dollars and potentially expose us to malpractice litigation.
Continuing to practice medicine the way we’ve been practicing it will cost us much more. Dr. Whitmore said firmly. Marcus Williams showed us that our expensive specialists can be catastrophically wrong. Either we learn from that revelation or we pretend it didn’t happen and wait for the next diagnostic failure to destroy more lives. The board voted unanimously to accept Dr. Whitmore’s resignation. But they also voted by a margin of 8 to four to implement her recommendations regarding Marcus Williams and the Chen family financial restitution.
As Dr. Whitmore cleaned out her office that afternoon, she felt something she hadn’t experienced in years. The satisfaction of having done the right thing, even when it cost her everything she had built her life around. Marcus Williams, meanwhile, was about to discover that sometimes losing everything is the first step toward finding what you were meant to do. 3 weeks later, Metropolitan Hospital unveiled the Marcus Williams Diagnostic Protocol, a revolutionary approach to medical consultation that would fundamentally change how the institution approached complex cases.
The protocol required that for any patient who had been unresponsive to treatment for more than 72 hours, a multiddisciplinary team would review the case from first principles, specifically including perspectives from non-traditional medical backgrounds. Dr. James Morrison stood before a packed auditorium of medical professionals, journalists, and hospital administrators from around the country to announce the new program. Behind him, a large screen displayed statistics that had shocked even him. In the 3 weeks since Marcus had begun consulting at Metropolitan, he had identified diagnostic errors in 11 cases, leading to successful treatment of patients who had previously been considered hopeless.
The Marcus Williams protocol, Dr. Morrison explained, is based on a simple but revolutionary premise. Medical expertise can come from sources beyond traditional medical education. Our new diagnostic team includes individuals who have studied medicine from personal necessity, who understand patient experience from having lived through misdiagnosis and who approach symptoms without the preconceptions that sometimes blind formally trained physicians. In the front row, Marcus sat beside Sophia Chen, both of them wearing the uncomfortable formal clothes that the hospital’s public relations department had insisted upon for the announcement.
Marcus clutched a new medical textbook, a gift from the hospital’s medical library. But Sophia noticed he still carried his original torn and taped book in his backpack. “The financial implications of this program are significant,” Dr. Morrison continued. “In 3 weeks, we’ve prevented an estimated two $3 million in unnecessary treatments and reduced average diagnostic time for complex cases by 60%. But more importantly, we’ve identified and corrected medical approaches that were actively harming patients. The audience stirred with interest.
Hospital administrators were always concerned about liability and cost control, but the suggestion that diagnostic errors were so common that a systematic review could prevent millions in wasteful spending was both encouraging and disturbing. The Marcus Williams protocol also includes a patient advocacy component, Dr. Morrison announced, “Every patient in our ICU now has access to a diagnostic review team that includes individuals who have personal experience with misdiagnosis. This team is empowered to challenge medical decisions and request alternative approaches when traditional treatments are failing.” Doctor Patricia Rodriguez, who had been promoted to head of the new patient advocacy program, stood to address the audience.
The most important change we’ve implemented is cultural. We’ve created an environment where observations from patients, family members, and non-traditional sources are valued equally with formal medical opinions. This requires humility from our medical staff, but it’s already saving lives. Marcus was invited to speak, though he had insisted that his remarks be brief and focused on practical applications rather than personal recognition. He approached the podium with his characteristic quiet confidence, looking out at an audience of medical professionals who represented the same institutional thinking that had failed his sister.
3 years ago, he began, “Doctors told me that my observations about my sister’s condition weren’t valuable because I didn’t have medical training. Today, those same types of observations are being used to save lives at one of the most prestigious hospitals in the country.” He paused, looking directly at several doctors in the audience who were taking notes on his comments. The difference isn’t that I learned more about medicine. The difference is that this hospital learned to listen to people who understand suffering, not just people who understand systems.
The applause was sustained and genuine. But Marcus raised his hand to continue. The Marcus Williams protocol isn’t about me. It’s about creating space for knowledge that comes from necessity, from experience, from paying attention to details that formal training sometimes overlooks. He gestured towards Sophia, who smiled encouragingly. Sophia is alive today because someone finally listened to what her body was trying to say. How many other patients are waiting for someone to listen to them? The question lingered in the auditorium long after the presentation ended, challenging every medical professional present to reconsider how they approached the fundamental act of healing.
One year later, the ripple effects of Marcus Williams’s intervention at Metropolitan Hospital had spread far beyond Chicago. Medical schools across the country were incorporating Williams protocols into their curricula. courses that taught medical students to value patient observations, family insights, and non-traditional sources of diagnostic information. Marcus himself had become something unprecedented in medical history, a credentialed diagnostic consultant who had never attended medical school. The American Medical Association had created a special certification category for individuals who demonstrated exceptional diagnostic abilities through practical application rather than formal education.
Marcus was the first person to receive this certification, but he wouldn’t be the last. He had moved into a small apartment near Metropolitan Hospital, but he still spent most of his nights walking through Chicago’s homeless communities, carrying his medical textbooks, and offering informal consultations to people who couldn’t afford traditional health care. The difference now was that he had institutional support. Metropolitan Hospital provided him with basic medical supplies and had established a fund to cover emergency treatment for the patients he identified.
Marcus, Dr. Trace Morrison said during one of their weekly meetings, “The board has approved funding for a national program. We want to establish Williams protocols in 20 major hospitals across the country. Are you ready for that level of responsibility?” Marcus looked up from the case files he was reviewing. Three patients from other hospitals whose families had contacted Metropolitan specifically requesting his consultation. “Dr. Morrison, I’ve been ready for this responsibility since the night Lily died. The question is whether the medical establishment is ready to admit that healing requires more than credentials.
Sophia Chen had become Marcus’ most effective advocate. Her recovery had been complete, but her experience as a conscious patient trapped in an unresponsive body had given her insights into medical care that she was determined to share. She had started a foundation called Lily’s Voice that connected families dealing with misdiagnosis to resources and advocates who could help them navigate medical systems. The hardest part, Sophia often told audiences at medical conferences, wasn’t being unable to move or speak. The hardest part was listening to doctors discuss my hopeless case when I knew I wasn’t hopeless.
Marcus gave me my voice back, but more importantly, he taught the medical system to listen. Dr. Elizabeth Whitmore had found her own path to redemption. After leaving Metropolitan, she had joined a free clinic on Chicago’s Southside, where she worked alongside Marcus to provide medical care to homeless populations. The experience had stripped away her professional arrogance and reconnected her with the reasons she had originally become a doctor. Working with Marcus taught me that I had been practicing medicine backward, she reflected during a documentary interview about the case.
I had been trying to fit patients into diagnostic categories instead of listening to what each patient was trying to tell me about their unique experience. The documentary titled Listening the Marcus Williams story had won an Emmy and sparked nationwide conversations about medical education, diagnostic accuracy, and the relationship between institutional authority and actual expertise. But Marcus’ most important legacy wasn’t the protocols, the certifications, or the national recognition. It was the simple practice of paying attention to patients, to families, to the details that formal training sometimes overlooked.
Late at night, when Marcus walked through the homeless camps beneath Chicago’s bridges, he still carried Lily’s photograph in his medical textbook. But now he also carried letters from dozens of patients whose lives had been saved by the diagnostic approaches that grief had taught him. “I kept my promise, Lily,” he whispered to her photograph on the anniversary of her death. No one else will die from the mistakes that killed you. Not if I can help it. Above him, the lights of Metropolitan Hospital glowed against the night sky, a symbol of institutional medicine that had learned to listen.
And in room 314, another patient was receiving care from doctors who understood that sometimes the most important medical knowledge comes not from textbooks, but from the simple act of remembering that healing begins with hearing what patients are trying to say. Marcus smiled, closed his textbook, and headed home to prepare for another day of proving that medicine’s highest calling isn’t about credentials or status. It’s about saving lives, one patient at a time.
News
“Blake Shelton Just SHUT DOWN Good Morning America — Walked Off Live After Tense Clash With George Stephanopoulos”
Blake Shelton STORMS Off Good Morning America After Explosive Clash With George Stephanopoulos — “You Don’t Get to Judge Me”…
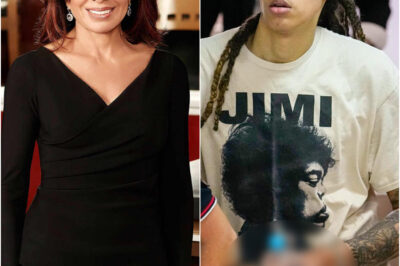
“SHOCKING: Pam Bondi Crushes Brittney Griner’s Olympic Dreams — A Historic Punishment No Athlete Has Faced Before!”
OH MY GOD! Pam Bondi Triumphs in Shocking Legal Battle Against Brittney Griner — Olympic Dreams Shattered in Historic Sports…
“How ‘South Park’ Destroyed Karoline Leavitt’s Image With Just One Necklace”
When a Cartoon Stripped the Cross: Karoline Leavitt, South Park, and the Fragility of Political Symbols In Washington D.C., even…
“Hollywood Silenced Keanu Reeves With One Question — And The Answer Terrified Everyone”
Keanu Reeves Sparks Media Firestorm After Off-Script Question Is Censored During Live Taping In an unprecedented moment that has stunned…
“BREAKING: Rachel Maddow Just Built a Secret News Empire — And She’s Bringing Colbert & Joy Reid Along for the Revolution”
Rachel Maddow, Stephen Colbert, and Joy Reid Launch Independent Newsroom — “The Maddow Project” Aims to Rewrite the Rules of…
“SHOCKING UPSET: Jeanine Pirro Blocks Brittney Griner From Olympics — The Heaviest Penalty in Sports History!”
Jeanine Pirro Triumphs in Stunning Legal Battle Against Brittney Griner — Landmark Ruling Sends Shockwaves Through Women’s Sports In a…
End of content
No more pages to load